Topic in Focus
Various Pathogens and the Effect of Vaccines
Illustration: Sisters of Design
Infectious diseases are caused by pathogens such as viruses, bacteria, fungi, or parasites. Vaccines are available mainly for diseases caused by bacteria or viruses. Viruses lead to, for example, polio, measles, rubella, or hepatitis. Bacteria cause diphtheria and tetanus. Many people in Germany are vaccinated against these diseases. Worldwide, vaccinations are also part of basic health care.
Researchers are trying to develop vaccines against dangerous pathogens. Their success depends also on the properties of the individual pathogen. Parasites, such as the pathogen that causes malaria (Plasmodium), can trick the human immune system. This single-celled organism has a highly complex structure and is able to re-adapt to the human host whenever it is put under pressure by drugs or vaccine candidates. To date, there is only one single vaccine approved for malaria (Mosquirix), and its protective effect is limited. The HI virus, which can cause the immunodeficiency disease AIDS, is also highly adaptable and variable. Such characteristics make it difficult to develop a vaccine. In contrast, suitable vaccines have been developed for poliomyelitis (polio), measles, and tetanus. In the case of tuberculosis, intensive work is being done on improvements since the available vaccine shows only poor efficacy on pulmonary tuberculosis.
“It works very well for childhood diseases like measles, mumps, and rubella. Here we are talking about viruses; they attack the body relatively quickly and cause an acute disease pattern. In case of an acute infection an immune response is mobilized, the body’s own defense system, which is generally successful if it intervenes quickly. Other clinical pictures are chronic, for example, tuberculosis, HIV/AIDS. You have it but cannot get rid of it as quickly, or sometimes not at all, which means that you are infected for life. You do not necessarily have to get sick right away, but you are nevertheless infected for life. This already indicates that, although an immune response is initiated, it is evaded or blocked, or some other mechanisms take effect – and the pathogens can persist despite ‘immunity’ and continue to survive in the body. Of course, it is more difficult to produce a successful vaccine against them because it would have to be better than our natural immunity. And there are actually only very few examples where this worked out, meaning to develop a vaccine that is better than what our natural immune response can do.”
“There is no vaccine for HIV because the virus is highly variable. Our studies have already shown that an infected person carries a swarm of viruses that already differ by 10 percent shortly after infection. That means, if you want to make a vaccine, you are shooting at a moving target, which is the first difficulty. And the second is that this infection is typically transmitted via the mucous membrane, and here you obviously need different defense barriers than with other infections that pass via the throat, for example. Making a vaccine that provides proper long-term protection has not been possible to date. It has been possible to create a certain immunity in the short term though. But in case of an infection that lasts a lifetime, where you can also get infected throughout your life, we must of course have long-term immunity. And that simply could not be achieved.”
“We now have a vaccine called Bacille Calmette-Guérin (BCG). It has been around for about a hundred years, and protects young children from violent cases of tuberculosis. That is very important. Unfortunately, it does not protect adults against the most common form of tuberculosis, which is pulmonary tuberculosis – the reason being that BCG is not much better than our natural immunity, the immunity caused by the infection. What we need is a new vaccine that is, first of all, better than the natural immunity against infection with the tuberculosis pathogen and also better than BCG. This is quite difficult, but in the last few years, some vaccine candidates have been developed. One of them by us, which is now in the last phase of clinical review, so it is being tested for protection against infection and disease in adults and young children.”
How does a vaccination work in the body?
Vaccines protect against infectious diseases by preparing the immune system for a pathogen. The vaccine simulates an actual infection by mimicking the virus or bacterium. Depending on the type and quality of the vaccine, the immune system reacts similarly to an actual infection: it begins to produce antibodies and immune cells. If one comes into contact with the pathogen after vaccination, the immune system recognizes it. The body’s own defense mechanisms are now quickly and specifically activated.
However, there are differences in how vaccinations work. Most vaccines approved to date produce high antibody titers, i.e., high antibody levels that neutralize pathogens. Viruses, for example, can be intercepted by antibodies and thus no longer penetrate the cells of the body. Infection is avoided, and the likelihood of infecting other people is reduced. However, with certain vaccines, the viruses still manage to penetrate the body’s cells and multiply despite vaccination. While symptoms are frequently observed here, they are less severe due to the trained immune system. As a result, the disease takes a comparatively mild course. Nevertheless, in such cases, vaccinated individuals can still pass on the virus. How infectious vaccinated individuals exactly remain depends, among other things, on the vaccine and the characteristics of the virus.
“There is a whole range of possibilities, and it depends very much on which strategy the pathogen has developed to settle and spread in the body. An easy one is still the example of vaccinating against a toxin. There we leave the pathogen completely alone and vaccinate only against the toxin. This is sufficient if the toxin is the only harmful feature of the pathogen. Examples are the classical vaccinations against diphtheria and tetanus. Another possibility is that the vaccination prevents pathogen attachment to the host cells. This is particularly important for viruses that cannot reproduce themselves but are reproduced by the host cell, i.e., by the body cell. If they cannot enter the cell, then sooner or later, their faith is sealed. They can no longer be reproduced, and therefore all die. There are many examples of such an infection with a virus, and SARS-CoV-2 is one of them. Here, you can block the pathogen, the virus, from attaching itself to the cell and sooner or later, it’s overridden.”
“One way would be that a vaccination induces antibodies that opsonize, which means more or less, making ‘palatable’. Bacteria like pneumococcus or meningococcus have a slippery capsule around them. Therefore, they cannot be taken up by phagocytes, which are there to eat bacteria and then kill them. The phagocytes cannot absorb them because they simply slip away. But once they are coated with antibodies, which bind to the capsule, the scavenger cell can recognize these antibodies. The bacteria is not slippery anymore and it will be eaten and dies. As I said, this is the case with pneumonia and meningitis, i.e. meningitis caused by meningococci or pneumonia caused by pneumococci. Another way is that you kill the cell that is replicating viruses, for example. Let’s say you have a virus; it managed to settle within a cell and replicates. If your immune system now recognizes: Attention, there are infected cells; we have to eliminate those cells, then this is also a way to kill the virus, because the virus is no longer replicated. Although we do have to sacrifice a few body cells this way, we will ultimately get through the infection better.”
Basically, three different types of vaccines exist: inactivated vaccines, live attenuated vaccines, and nucleic acid-based vaccines. In the case of inactivated vaccines, killed pathogens or fragments thereof are administered. These are sufficient to activate the immune system. Such vaccines must be refreshed because the body does not form an immunological memory. In the case of live attenuated vaccines, the body is given attenuated pathogens, for example, viruses, that can no longer cause the disease. The immune system nevertheless recognizes them as invaders and develops defense strategies. In addition, the body forms memory cells that recognize the pathogen when it invades again and that already know how to fight it. Live attenuated vaccines, such as the measles vaccination, therefore usually have a lifelong effect.
Genetic information as the basis for novel vaccines
For several years, fundamental research has been conducted on another type of vaccination: nucleic acid-based vaccines. The novelty of these vaccines compared to vaccination with conventional dead or live attenuated vaccines is that they do not contain pathogens or pathogen components which directly trigger an immune response. Instead, they are based on the genetic information of the pathogens. This new vaccine category includes mRNA and DNA vaccines as well as vector vaccines.
In the case of mRNA and DNA vaccines, the direct “blueprint” for components of the pathogen (messenger ribonucleic acid, mRNA) or the carrier of genetic information underlying this blueprint (deoxyribonucleic acid, DNA) is introduced into the cell. According to this “blueprint”, the cell produces a protein of the pathogen, which then triggers the immune response. The immune system produces soluble defense substances, the antibodies, and forms specific T cells, each of which is directed against the pathogen protein. If a vaccinated person subsequently comes into contact with the pathogen, the immune system recognizes it by its characteristics and can combat it. Several mRNA vaccines against COVID-19 were first approved in 2020. The mRNA cannot be incorporated into the human genome because the conversion of RNA to DNA is not possible within human cells.
Vector vaccines use so-called gene shuttles (vectors) as a “means of transportation”. These genetically modified viruses transport the gene, i.e., the DNA for the respective pathogen component, into the cells. According to current knowledge, the viral vectors used for vaccination are harmless to humans and cannot cause disease. Vector vaccines are used against dengue fever and Ebola fever.
“A particularly attractive technical feature of these vaccines is that an RNA, which is made up of only a few basic building blocks assembled in different ways, can be produced very, very quickly. RNA vaccines can therefore be used to create a vaccine against a particular tumor in a specific person. And that was actually the starting point of these RNA vaccines. Then, suddenly, a new pathogen emerged, SARS-CoV-2, and clever people immediately took this method to develop RNA vaccines against it and to protect us from COVID-19, because they were able to make the modification quickly. The new thing is that we do not use the actual antigen, the protein, but rather the information, which is RNA. It is also important to note that RNA is not able to integrate into our genetic material. It cannot incorporate into the genome and is therefore not carried on over a lifetime or maybe even into the next generation. We can rule that out as well.”
Challenge posed by mutations
One challenge in combating infectious diseases is mutations, by which the pathogen adapts to the host organism by changing its genetic material and characteristics. Thus, the immune system cannot recognize the pathogen anymore and an immune response is not initiated. For research, this means that the vaccine may also need to be adapted. This happens, for example, every year with the flu vaccination. Influenza viruses are highly mutable. The World Health Organization (WHO) collects all relevant data on the properties of the globally circulating variants and makes them available to all countries.
“Mutations are first of all something quite normal and not necessarily disturbing. Nevertheless, they can disturb a vaccination effect if the mutation occurs at the exact point the vaccination is aimed at, or rather, where the antibodies are aimed at. Immunity through antibodies is quite precise; the antibodies recognize only a very small part of the pathogen or its antigen. And if that has changed, the antibody may not attack properly. Ultimately, a mutation is problematic for us if it allows the pathogen to evade our defenses. A good example would be the seasonal flu. I mean the kind of flu that hits us year after year and which we have to get newly acquainted with every year. It always changes just a little bit, but the changes are so distinct that last year’s vaccine is no longer able to recognize this year’s pathogen. And therefore, we always have to adapt our vaccines.”
“The flu pathogens have a much more dangerous trick up their sleeve. Namely, they can engage in an exchange with each other. So, let’s say two influenza pathogens happen to collide in a pig somewhere in East Asia. They are able to exchange entire parts of their genetic material with each other, and then a completely new strain of influenza emerges. This is the cause of the so-called pandemic flu, which we have already seen in the past, e.g. the Spanish flu of 1918 and later the Asian flu or the Hong Kong flu, which happened not that long ago, about 50 years. Those were major changes, and at least back then, people couldn’t come up with a new vaccine right away, and that’s when the pandemics happened.”
Self-protection and community protection
A vaccination initially protects the vaccinated person from infection and disease. As soon as a large number of people is vaccinated, each individual vaccination also helps to protect others. For example, chronically ill people or patients after an organ transplant depend on the risk of infection being reduced for them, as they either cannot get vaccinated themselves or do not build up sufficient immune protection after vaccination.
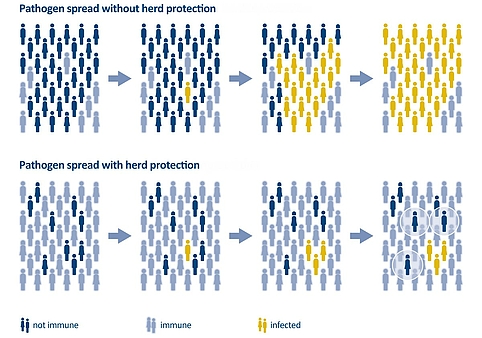
Vaccination can induce herd immunity or rather herd protection, which is an important aspect of community protection. The aim is to prevent the pathogen from spreading further, since enough people are already immune – either because they have been vaccinated or have already recovered from the disease. If this is true for a large percentage of the population, herd protection is achieved. The percentage rates vary depending on the pathogen and its characteristics: for diphtheria, for example, it is sufficient if more than 80 percent of the population is immune, whereas, for measles, community protection is effective at a rate of around 95 percent.
Figure 1: Schematic representation of the spread of a pathogen in the population without and with herd protection. People who cannot be vaccinated are only protected by the vaccinated in their environment if the majority of the population is immune to a pathogen. If, on the other hand, the proportion of immunity in the population is too low, the pathogen can spread more easily. Source: BZgA | Illustration: Emde Grafik
Difficulties arise when it is unclear whether a vaccine can also prevent infection, i.e., to what extent vaccinated individuals can still become infected or transmit a pathogen. If vaccinated individuals continue to spread a pathogen, protection for the unvaccinated cannot develop through vaccination of the population.
Successes against infectious diseases
To date, there is one human disease that has been completely eradicated through vaccination: smallpox, which is transmitted by the variola virus (VARV). The last major epidemic broke out in Germany around 1870, causing the deaths of around 170,000 people. In the fight against smallpox, a vaccine in the narrower sense of the word was used clinically for the first time in England around 1800. Country doctor Edward Jenner observed that people who had been infected with cowpox before did not become ill, or only slightly ill, when later infected with human smallpox. Accordingly, he transferred tissue material from cowpox lesions to humans. Subsequently, vaccines were developed that contained the isolated cowpox viruses (vaccinia viruses). In 1967, the World Health Organization (WHO) made smallpox vaccination mandatory worldwide, and in 1980 the virus and smallpox were officially declared eradicated.
Polio has also been nearly eradicated worldwide. The last case in Germany was registered in 1990. Europe is considered polio-free by the WHO, no cases were reported after 1992. However, polioviruses still circulate in Pakistan and Afghanistan and could spread from there to other regions. Therefore, vaccination against poliomyelitis continues. Similarly, measles, one of the most contagious diseases of all, has declined in many world regions thanks to vaccination. Thanks to a high vaccination rate, the number of tetanus cases in Germany is also very low. In developing countries, however, many people still contract tetanus.
“So far, we have only succeeded once in the case of smallpox. Smallpox vaccination was so successful that it ultimately led to the eradication of the disease. It must be said, though, that this was only possible because, as the name suggests, human smallpox only affects humans. As with all pathogens that can hide out in animals, i.e. have a second or third reservoir such as the SARS viruses in bats and other animals, eradication will be much more difficult to achieve. Because here, you would also have to be able to somehow eliminate those reservoirs. The second example that impresses me very much is, of course, the near eradication, or at least the clear control, of polio. The polio vaccine has actually pushed the polio pathogen back so far that there are only very few niches where it still persists. This is Afghanistan and Pakistan at the moment.”